Harnessing and accelerating the regenerative capacity of the pancreas is already a promising research project that joins the pharmacological revolution.
Although it may be socially misinterpreted as “benign ,” the truth is that diabetes is a chronic disease with serious health consequences. It’s a threat that affects more than five million adults in our country , a figure that has increased by 42% in Spain since 2019.
Fortunately, and thanks to tireless medical and scientific work, there is increasingly more good news for people with diabetes, as was made clear this week during the 36th National Congress of the Spanish Diabetes Society Foundation (FSED) . Proof of this is that it is no longer unreasonable to talk about a cure for diabetes, thanks, for example, to the pancreas’s innate ability to regenerate , even decades after the onset of diabetes. This is the strategy followed by the research group of Professor Juan Domínguez Bendala , director of the Pancreatic Regeneration and Stem Cell Laboratory at the Diabetes Research Institute at the University of Miami , which is already yielding promising results and involves enhancing a natural mechanism of the pancreas.
“Transplanting beta cells (whether islets from a donor or differentiated stem cells) is a promising approach that will very likely lead to effective therapies in the short term . But it is still a brute force approach to the problem ,” says the researcher, who argues that ” if we were to harness the natural regenerative capacity of the pancreas, accelerating it in a controlled manner, the result would be much more like a cure . ” Thus, the development of strategies aimed at accelerating this process could lead to the functional recovery of beta cells in insulin-dependent patients (especially those with type 1 diabetes).
Regenerative capacity
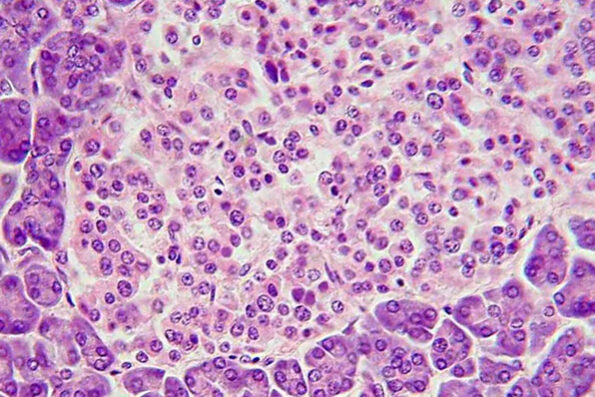
Specifically, this group of researchers has found progenitor cells in the pancreas capable of regenerating islets in both newly diagnosed patients and those who have had diabetes for decades. In principle, the strategies they are developing should be applicable to all patients who lack a sufficient functional mass of beta cells. Transplantation of islets obtained from donors has already been approved by the FDA (the US regulatory body), and transplants of islets generated from stem cells are in advanced stages of clinical trials. ” These advances in cell therapies will build a bridge toward regenerative therapies like the one we are developing (still in the research phase), which would not require a transplant of any kind . The impact of these therapies on patients’ quality of life can be considered transformative ,” acknowledges Domínguez Bendala.
The key lies in the use of a growth factor that has been used in clinical practice for decades and has proven safe and effective for other applications. “It’s bone growth factor 7, BMP-7 , capable of selectively activating the controlled proliferation of pancreatic progenitor cells and their differentiation into beta cells. And all of this within the organ, stimulating the same process that led to its development and which is naturally reactivated in situations of pancreatic stress ,” explains the researcher, who acknowledges that “it remains to be established whether the new cells regenerated in this way will also be rejected by the immune system, as there are arguments for and against, but this can be clarified in other phases of research. However , assuming the worst-case scenario, our approach could be combined with strategies that reduce the virulence of the autoimmune attack.”
Author: Raquel Bonilla
Date: Created: 04/27/2025 09:00
Last updated: 04/27/2025 09:00
Source: Larazon.es
Link: https://www.larazon.es/salud/cada-vez-mas-cerca-cura-diabetes_20250427680dd604e52da91ed5311529.html
Note: The Nutrigenomics Institute is not responsible for the opinions expressed in this article.
PHOTO FROM WIKIPEDIA.